The issues
The quality of patient care depends on producing and analysing results in order to improve diagnosis and provide appropriate treatment. But in sub-Saharan Africa and developing countries in general, patients have very limited access to biological monitoring and additional testing, because laboratories are poorly equipped and medical staff are insufficiently trained in the use of the available laboratory equipment.
Our priorities
- Improve diagnoses
- Provide all patients with access to quality biological monitoring
Our objectives
- Ensure that staff in technical facilities and laboratories have access to adequate tools and are properly trained in diagnosing and monitoring patients
- Strengthen the link between technical facilities and other health services to ensure that test results lead to optimal patient care
What we do in the field
Improving national strategies and policies
- Advocate for better access to additional tests (biological, imaging), particularly their integration into the minimum healthcare package
- Support development of standards and procedures: screening algorithms, best practices guides
Training
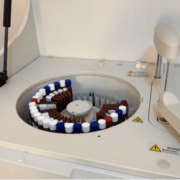
- Train and mentor technicians in using technology and managing technical facilities: tools to help with diagnosing opportunistic infections, verifying CD4 counts, measuring viral load, genotyping
Advising on organisation and coordination
- Improve coordination between actors in technical facilities and clinical services (tutoring, organising medical staff)
- Support the establishment of sampling rounds and result reporting
Infrastructure and equipment
- Support equipment acquisition and laboratory refits
- Support equipment inventory management and maintenance-plan monitoring
Testimonial
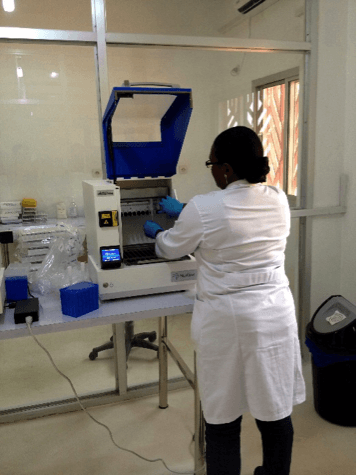
In the laboratory we perform HIV-specific screenings and tests such as CD4 count or viral load determination. This biological monitoring is essential for adjusting treatments—Biologist at the National Laboratory Reference
One of the challenges of HIV management in Sierra Leone is to keep patients in the healthcare system and avoid losing sight of them. Some will stop coming for their appointments once they have been screened or treatment has begun.
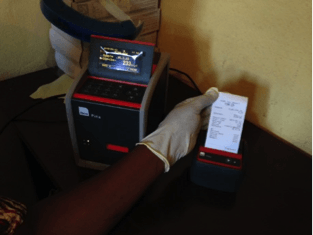
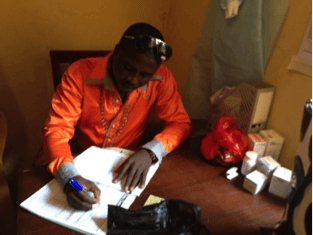
As part of a pilot project developed at the Lumley secondary hospital in Freetown, Solthis equipped this facility with a CD4 counter and trained a laboratory assistant to use it. Patients who have tested positive can now have on-the-spot CD4 counts and immediate adapted ARV treatment after appropriate counselling. Patients thus receive treatment quickly, are given a better understanding of the challenges of the illness and its treatment, and are more likely to remain in the system.
As shown in these photos, patients who test positive for HIV have the option of receiving an immediate CD4 count. A patient with a count higher than 350/mm3 can begin adapted ARV treatment right away.
In a single morning, a patient who has tested positive begins receiving care, and as such is more likely to remain in the system.
Solthis has developed specific tools to assist with biological, immunological and virological monitoring, such as the user's manual for the PIMA test and the guide on manual extraction for viral load measurement.
Through the OPP-ERA project, Solthis enabled Guinea to provide HIV viral load tests for the first time in public health structures. Viral load measurement is essential for monitoring ARV patients to ensure adequate treatment and detect treatment failure.
This project is funded by UNITAID and implemented by a co-funding consortium of French partners (FEI, ANRS, ESTHER, Sidaction and Solthis) in four countries: Burundi, Cameroon, Ivory Coast, and since March 2013, Guinea. OPP-ERA project [French only].
| Our national partners | Our collaborations |
|
|